What Is Post-Herpetic Neuralgia?
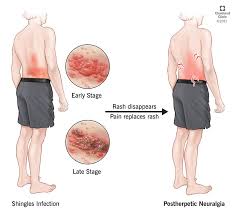
Post-herpetic neuralgia (PHN) is a chronic pain condition that occurs as a complication of shingles, a viral infection caused by the varicella-zoster virus. After a shingles outbreak resolves, some individuals experience persistent nerve pain in the affected area, which can last for months or even years. PHN is one of the most common and debilitating complications of shingles, especially in older adults.
Causes and Risk Factors of Post-Herpetic Neuralgia
Understanding the Role of the Varicella-Zoster Virus
PHN Post-herpetic neuralgia develops when the varicella-zoster virus damages the nerves during a shingles outbreak. This nerve damage disrupts the normal communication between nerves and the brain, leading to chronic pain.
Key Risk Factors
- Age: Individuals over 60 are more prone to PHN.
- Severity of Shingles: A severe rash or intense pain during the shingles infection increases the likelihood of PHN.
- Delay in Treatment: Untreated or delayed antiviral therapy can exacerbate nerve damage.
- Weakened Immune System: Conditions such as HIV, cancer, or the use of immunosuppressive medications heighten the risk.
Symptoms of Post-Herpetic Neuralgia
Persistent Pain
PHN is characterized by a burning, stabbing, or aching pain that persists for more than 90 days after the shingles rash has healed. The pain is often localized to the area where the rash appeared.
Heightened Sensitivity
- Allodynia: Pain triggered by stimuli that normally wouldn’t cause discomfort, such as a light touch or clothing.
- Hyperalgesia: An exaggerated response to painful stimuli.
Other Symptoms
- Tingling or numbness in the affected area.
- Itching that feels deep and unrelenting.
- Fatigue or sleep disturbances due to chronic pain.
Diagnosis of Post-Herpetic Neuralgia
Diagnosis is primarily based on a patient’s medical history and symptoms. A doctor may ask about:
- The timeline of the shingles infection.
- The location and nature of the pain.
- Any other ongoing medical conditions.
No specific tests exist for PHN, but ruling out other conditions through imaging or nerve studies may be part of the diagnostic process.
Treatment Options for Post-Herpetic Neuralgia
Medications
- Anticonvulsants
Drugs like gabapentin and pregabalin are commonly prescribed to reduce nerve pain and improve sleep. - Antidepressants
- Tricyclic antidepressants, such as amitriptyline and nortriptyline, help by altering pain signals in the brain.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs) may also provide relief.
- Topical Treatments
- Lidocaine Patches: These provide localized pain relief by numbing the affected area.
- Capsaicin Creams: Derived from chili peppers, capsaicin desensitizes overactive pain receptors.
- Pain Relievers
- Over-the-counter NSAIDs (e.g., ibuprofen) or prescription-strength opioids may be used for severe pain.
Nerve Blocks and Injections
For individuals with refractory PHN, local anesthetic nerve blocks or steroid injections can provide temporary relief.
Alternative Therapies
- Acupuncture: This may help improve nerve function and reduce pain.
- Transcutaneous Electrical Nerve Stimulation (TENS): Uses electrical pulses to disrupt pain signals.
- Cognitive Behavioral Therapy (CBT): Addresses the psychological impact of chronic pain.
Preventing Post-Herpetic Neuralgia
Shingles Vaccination
The shingles vaccine is the most effective way to reduce the risk of both shingles and PHN. Vaccines like Shingrix are recommended for adults over 50, providing strong protection against the varicella-zoster virus.
Early Antiviral Treatment
Starting antiviral medications (e.g., acyclovir, valacyclovir, or famciclovir) within 72 hours of a shingles outbreak can significantly lower the risk of PHN.
Living with Post-Herpetic Neuralgia
Coping Strategies
- Pain Management Plans
Collaborate with healthcare providers to develop a personalized pain management strategy. - Lifestyle Adjustments
- Wear soft, loose clothing to minimize skin irritation.
- Practice relaxation techniques such as meditation or yoga to manage stress.
- Support Systems
Join support groups or seek counseling to cope with the emotional challenges of living with chronic pain.
The Impact of Post-Herpetic Neuralgia on Quality of Life
PHN can disrupt daily activities, relationships, and mental health. Chronic pain may lead to depression, anxiety, and social isolation. Therefore, a holistic approach to treatment—addressing both physical and emotional well-being—is essential.
Research and Advancements in Post-Herpetic Neuralgia
Ongoing studies focus on:
- Novel Medications: Exploring new drug formulations to target nerve pain more effectively.
- Gene Therapy: Investigating ways to repair damaged nerve tissue.
- Personalized Medicine: Tailoring treatments based on genetic factors to enhance efficacy.
Conclusion
Post-herpetic neuralgia is a complex and often debilitating condition, but early intervention, effective treatment, and preventive measures can significantly improve outcomes. Individuals experiencing PHN should seek medical advice promptly to address their symptoms and improve their quality of life.